In the 18th century, a French man named François Bossier de Lacroix became the first person ever to be credited with systematically classifying diseases. Now, in 2019,...
The theme of this year’s National Health Center Week (NHCW) is Community Health Centers: Lighting the Way for Healthier Communities Today and in the Future. The goal of NHCW is to create public awareness of health center programs and the work they do. Now, more than ever before, it’s important to recognize the value community health centers (CHCs) provide to local populations, especially those who are vulnerable or underserved.
Federally qualified health centers (also called community health centers) across the nation help over 28 million patients by providing high-quality, cost-effective care in medically underserved areas. The centers usually offer integrated services in areas such as medical, dental, and behavioral health, based on the community’s unique needs. The populations who utilize health centers usually live below the poverty line, and are more likely to experience complex and underlying health issues. Health centers accept all patients with or without insurance, which helps reduce emergency department costs in hospitals.

This is the right time to be advocating for increased resources for CHCs. Health centers are not only experiencing an overwhelming increase in patients, but they’re also getting hit with the financial strain that comes with such a damaging pandemic, as all attention has been focused on COVID-19. According to the National Association of Community Health Centers (NACHC), health centers have lost upwards of $7.6 billion in revenue during the pandemic. And on a personal level, CHC workers trying to keep themselves healthy while treating their patients, which is no small task.
With federal officials relying on these centers to respond to COVID-19, community health centers’ importance is even more apparent, alongside their reputation for being the go-to destinations for primary care in their communities. Community health centers have unfortunately seen a scarcity of patients who are in need of any kind of care other than COVID-19 treatment. With patients refraining from seeking regular care, these health centers are feeling the loss of a major source of income: their patients.

Community health centers rely on federal subsidies for about 20% of their revenue. Most of this is from the Community Health Center Fund, which was established under the Affordable Care Act. This fund is not a reliable source, as it has been getting renewed for mere months at a time, and is set to expire in November 2020. This means that community health centers need our advocacy for Congress to decide to continue to support these centers.
In order serve the growing need for health and social services in their communities, health centers also need increased funding and expedited health center payments. With the increase in the utilization of healthcare technologies such as telehealth due to COVID-19, community health centers are struggling to keep up with these modern requirements, as they do not have the financial resources to invest in these new technologies that would allow them to better serve their communities.
The association's advocacy toolkit offers resources from letter templates to enlist new allies and advocates, to content to spread awareness of the need for community health center support.
Community health centers are involved in nearly all of the community care networks supported by Activate Care. This is one of the reasons why we feel so strongly about the importance of CHCs in our safety net. We have seen firsthand the critical role of care coordinators in these organizations. It's also important to note that most CHCs – 59% of them, according to NACHC – are recognized as Patient-Centered Medical Homes (PCMH) which comes with care coordination service requirements.
It is critical that PCMHs have the resources needed to accomplish care coordination activities. Traditional fee-for-service reimbursement only pays for face-to-face visits. According to AHRQ, a recent study of high-functioning primary care practices found that in addition to seeing an average of 18 patients, physicians also handle an average of 24 telephone calls, 17 emails, 12 prescription refills, and 45 reviews of laboratory, imaging, or consultation reports per day. Requiring additional activities without compensation is unlikely to result in increased care coordination.
We will explore this and other current issues related to care coordination in our upcoming SDOH MasterClass webinar, A Day in the Life of a Care Coordinator. Hosted by my colleague Brooke Sabia, a recent care coordinator, please join us to hear her stories about surviving in her role without, and then flourishing with, care coordination tools from Activate Care.
In the 18th century, a French man named François Bossier de Lacroix became the first person ever to be credited with systematically classifying diseases. Now, in 2019,...
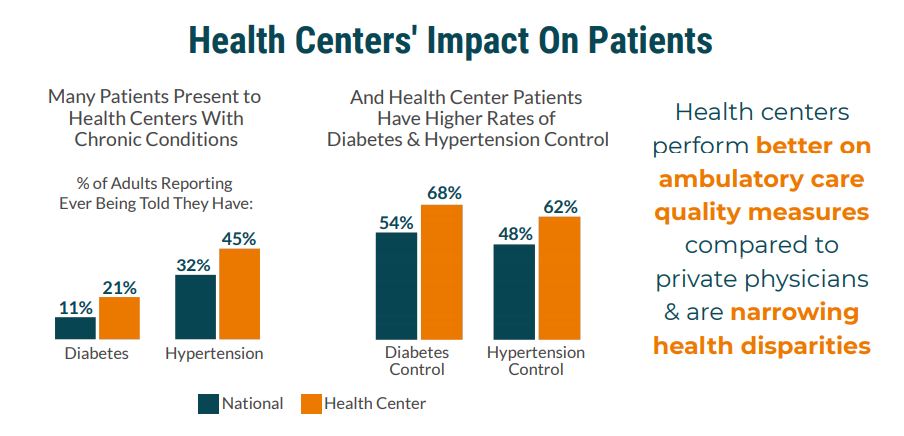
Why do America's community health centers work so well? They provide high-quality health care, improve health outcomes, and narrow health disparities, even while serving...