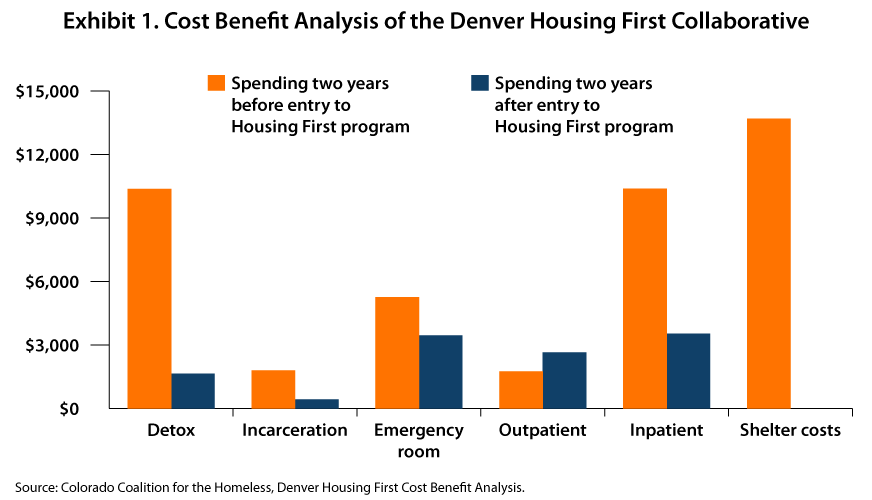
In 2018, the Colorado Coalition for the Homeless (CCH) granted a $2.4 million dollar expansion to the “Housing First” model that they have already been using for two...
When you hear scientists and researchers talk about COVID-19 now, you get a strong sense of how much we have learned about the virus in such a short time.
“The majority of people who have COVID-19 are out in the community, and they are either asymptomatic or only mildly ill,” said Dr. Sulggi Lee, a UCSF assistant professor of medicine, in the UCSF magazine. But for those who do experience symptoms, they can be a bewildering array of health challenges: loss of smell and taste; nausea or diarrhea; arrhythmias or heart attacks; damage to kidneys or livers; headaches, blood clots, rashes, swelling, or strokes.
We thought it was just a respiratory virus - but it’s much stranger than that, and it can last for a long time.
In this post:
A recent study in the US found that only 65% of people had returned to their previous level of health 14-21 days after a positive test. While most patients will recover spontaneously by getting treatment for their symptoms, along with enough rest, all are at risk of long-term complications.
Long-term complications are part of the condition now called post-acute COVID-19 or “long COVID”, which appears to be a multisystem disease that can impact our physical, mental, and social health and well-being. These lingering effects could come from the virus itself, the inflammation it triggers, or complications stemming from hospitalization or isolation.
With school closures, a large number of families out of work, and the need for social distancing, the pandemic has worsened long-term social challenges like food insecurity, homelessness, and unemployment. According to Dora Barilla, Group Vice President for Community Health Investment at Providence St. Joseph Health, 12% of Americans now live in households where someone didn’t have enough to eat in the last 7 days.
Health systems across the country have launched COVID-19 rehabilitation and recovery programs, to serve as a medical home for patients with myriad complications who require coordinated care. These patients often require care from a gamut of specialists, including pulmonologists, cardiologists, neurologists, rheumatologists, and psychiatrists. While some patients in these recovery programs never went to the hospital for treatment, others had a long hospital stay, followed by inpatient rehabilitation.
At the heart of this approach is the provision of whole person care that not only cuts across disciplines, but also across sectors using centralized expertise through virtual multidisciplinary clinics. In addition to harnessing the resources available within a single health system, coordinated care strategies also call for community-based, cross-sector collaborations that unify healthcare and social services around the needs of long COVID sufferers.
Several health systems are making progress in these areas:
Mount Sinai Center for Post-COVID Care, NY
New York City’s first long COVID clinic was launched at Mount Sinai Hospital in May 2020, serving as a hub for patients to access comprehensive multi-specialty care and systematic evaluation of the long-term impact of COVID-19. A personalized treatment plan is offered to all patients, incorporating expertise from primary care, pulmonary medicine, cardiology, infectious disease, nephrology, physiatry, physical and occupational therapy, radiology, neuropsychiatry, behavioral health, social work, and pharmacy.
UTHealth COVID-19 Center of Excellence, TX
The first post-acute COVID clinic in Houston was formed by clinicians and researchers at UTHealth in September 2020, who are working together to help both adults and children who are still suffering from the effects of the disease. The team has also received NIH funding to identify disease hotspots and testing deserts in three racially diverse areas across Houston, and then develop and evaluate intervention strategies to increase COVID-19 testing.
UCHealth Post-COVID ICU Clinic, CO
The University of Colorado’s Post-COVID ICU Clinic, led by Dr. Sarah Jolley, brings together specialists in pulmonology, cardiology, pulmonary rehabilitation, physical and occupational therapy, and behavioral health to work with patients they call “long-haulers”, whose symptoms linger for more than a month after recovery. The clinic has a virtual care model in place which has providers collaborating to assess each patient remotely and consult with one another to decide on an appropriate plan of care.
Northwestern Neuro COVID-19 Clinic, IL
According to Northwestern Medicine’s Dr. Igor Koralnik, at least one-third of people who have COVID-19 experience neurological complications. The Neuro COVID-19 Clinic provides care for these side effects while studying the long-term effects that COVID-19 has on the brain, nervous system and muscles. Patients access a telehealth-enabled care team drawing from experts in the Northwestern Medicine Neuroinfectious Diseases Program.
Keeping COVID-19 patients from falling through the cracks in the healthcare system takes concentrated effort, especially when staff and resources are constrained. Since the start of the pandemic, Activate Care has made our cloud-based COVID-19 care coordination tools available at no cost to any community needing support for their COVID-19 response strategy.
Activate Care’s COVID-19 Response Platform is designed to capture all of COVID cases and discharges into a shared database, allowing your team to conduct outreach and contact after discharge as needed. The platform is telehealth-enabled and can be configured to support patient education and self-management efforts.
Counties and care teams across the country have leveraged the COVID-19 Response Platform to support active management of COVID-19-positive individuals. In Humbold County, CA, it was implemented in less than a week and is now used for rapidly housing at-risk homeless individuals in motels; it provided the care coordination framework for the newly housed and was described as a “major success” by the California Health Care Foundation.
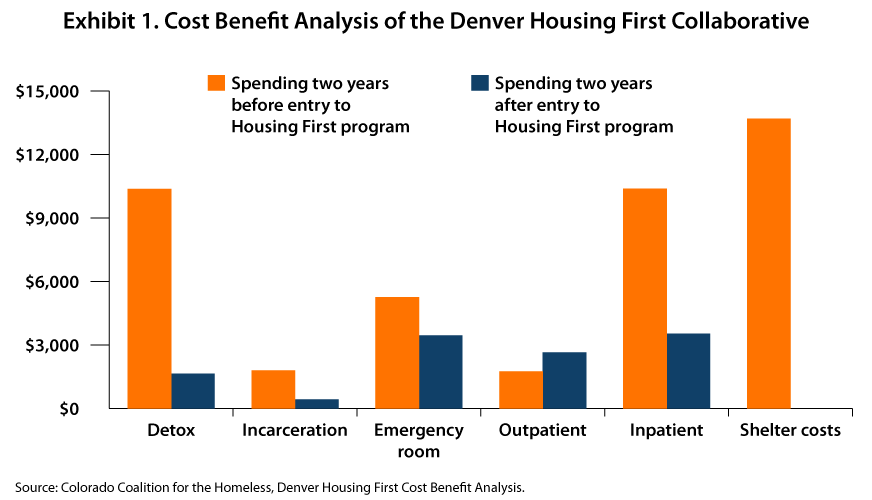
In 2018, the Colorado Coalition for the Homeless (CCH) granted a $2.4 million dollar expansion to the “Housing First” model that they have already been using for two...

Community information exchange*, or CIE, is a community-based strategy for improving the delivery and integration of healthcare and social services. As its name...