In the 18th century, a French man named François Bossier de Lacroix became the first person ever to be credited with systematically classifying diseases. Now, in 2019, the classification of patient conditions has been expanded to a standardized index that allows our healthcare system to efficiently categorize patient needs and accurately bill for services delivered, with just a seven-character code sequence.
How are medical billing codes organized?
Today, medical billing codes are governed by the ICD, or the International Statistical Classification of Diseases and Related Health Problems, a medical classification list managed by the World Health Organization. The ICD is in its tenth revision, published in 1994, and so is often referred to as ICD-10. The United States uses two variations of ICD-10:
ICD-10 Clinical Modification (ICD-10-CM), with over 68,000 diagnosis codes used for specifying diagnoses and classifying morbidity.
.png?width=600&name=ICD-10-CM%20example%20(2).png)
ICD-10 Procedure Coding System (ICD-10-PCS), with over 87,000 procedure codes used for classifying procedures performed in hospital inpatient healthcare settings.
.png?width=600&name=ICD-10-PCS%20example%20(1).png)
Why are billing codes important to SDOH-informed care models?
Since its global adoption, the ICD is used for much more than just a list of diseases. Physicians in the US use ICD-10-CM codes to specify exactly what diagnosis the patient has, and then use ICD-10-PCS codes to bill the patient and insurers for the procedures delivered. The codes can also be used to track the spread of diseases and even evaluate how social determinants of health (SDOH) affect patient conditions.
SDOH come into play in the often-overlooked Z section of the ICD-10-CM codes. The Z category for ICD-10-CM codes represents “factors influencing health status and contact with health services”, including genetic markers, previous interactions with the health system, problems relating to education, etc.
Insurance claims for certain Z codes have been marked by insurance companies as ‘zero balance claims’. Zero balance claims are claims that are paid on a per member per month basis but do not include repeat instances. For example, the insurance company will reimburse a social service for helping a patient, but only at a flat rate, not for each individual occurrence.
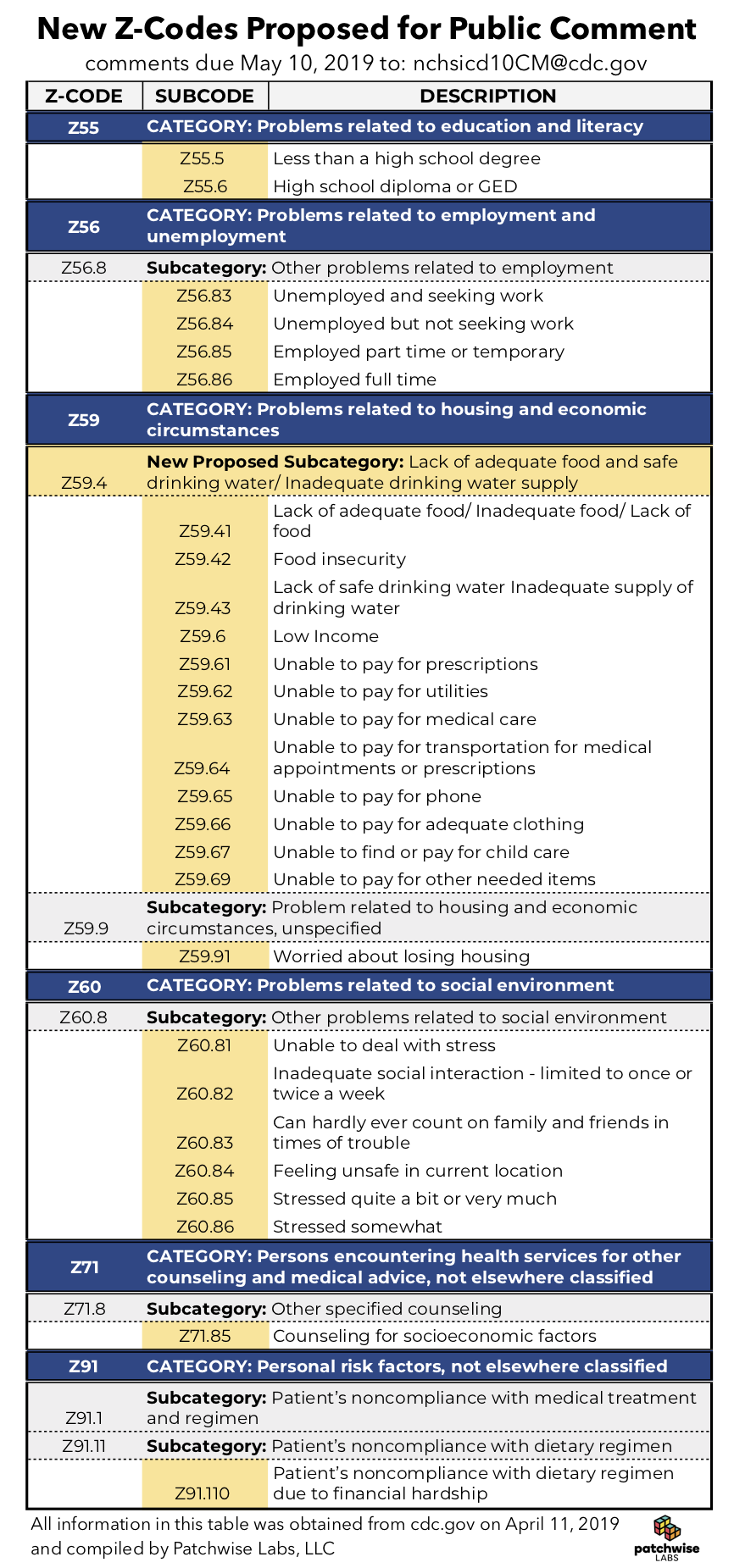
This type of payment model has existed for a long time, but more recently it is being used to track SDOH data among the patients using care coordination services. Insurance companies and hospitals can identify the high cost patients using this payment plan and evaluate how to help them. The ICD governing authorities have been contemplating the expansion of Z codes to more accurately capture social interventions for patients and families, which will help with efforts to integrate social services into local healthcare systems. The proposed codes are as follows:
Recording SDOH data helps health systems know what outside factors are influencing their patients beyond the care they are providing for them. Currently, the use of Z codes has not become commonplace in outpatient data because reimbursement systems do not currently incentivize clinics and hospitals to record such detailed descriptions. Although, as more data is collected and analyzed, Z codes are showing more promise in the field of health analytics.
