
One of my most memorable rotations during medical school was a month-long pairing with a late-career general practitioner. He had been using the traditional written...
We look to the social determinants of health (SDOH) to predict why a community is unhealthy. They challenge the notion that health is something primarily determined by healthcare services delivered and the absence of illness or disease. Research by County Health Rankings shows us that only 20 percent of health is determined by traditional healthcare. In comparison, the remaining 80 percent is determined by factors like housing stability, food security, and employment opportunities - the social determinants of health.
In 2005, the World Health Organization defined SDOH as “the conditions in which people are born, grow, live, work, and age.” Since then, many nuances in definitions have emerged, which speaks to the complexity and challenge of establishing a consensus approach to population health issues. The Kaiser Family Foundation has helped make SDOH more actionable by identifying the domains that drive the majority of health outcomes, including economic stability, neighborhood and physical environment, education, food, community and social context, the healthcare system, and policy. Communities are healthy when they can address these domains by ensuring access to quality schools, good-paying jobs, healthy foods, quality healthcare, affordable housing, and safe neighborhoods. When communities lack these resources and opportunities, the health of a community suffers.
As a recent MPH graduate of Saint Louis University’s College of Public Health and Justice, the social determinants are fully ingrained in my perspective on health. Public health offered me a framework to understand and intervene on the social determinants of health and health equity across the life-course. The Social-Ecological Model (SEM), one of the first models I learned in my studies, reveals the complexity of understanding and addressing public health issues.
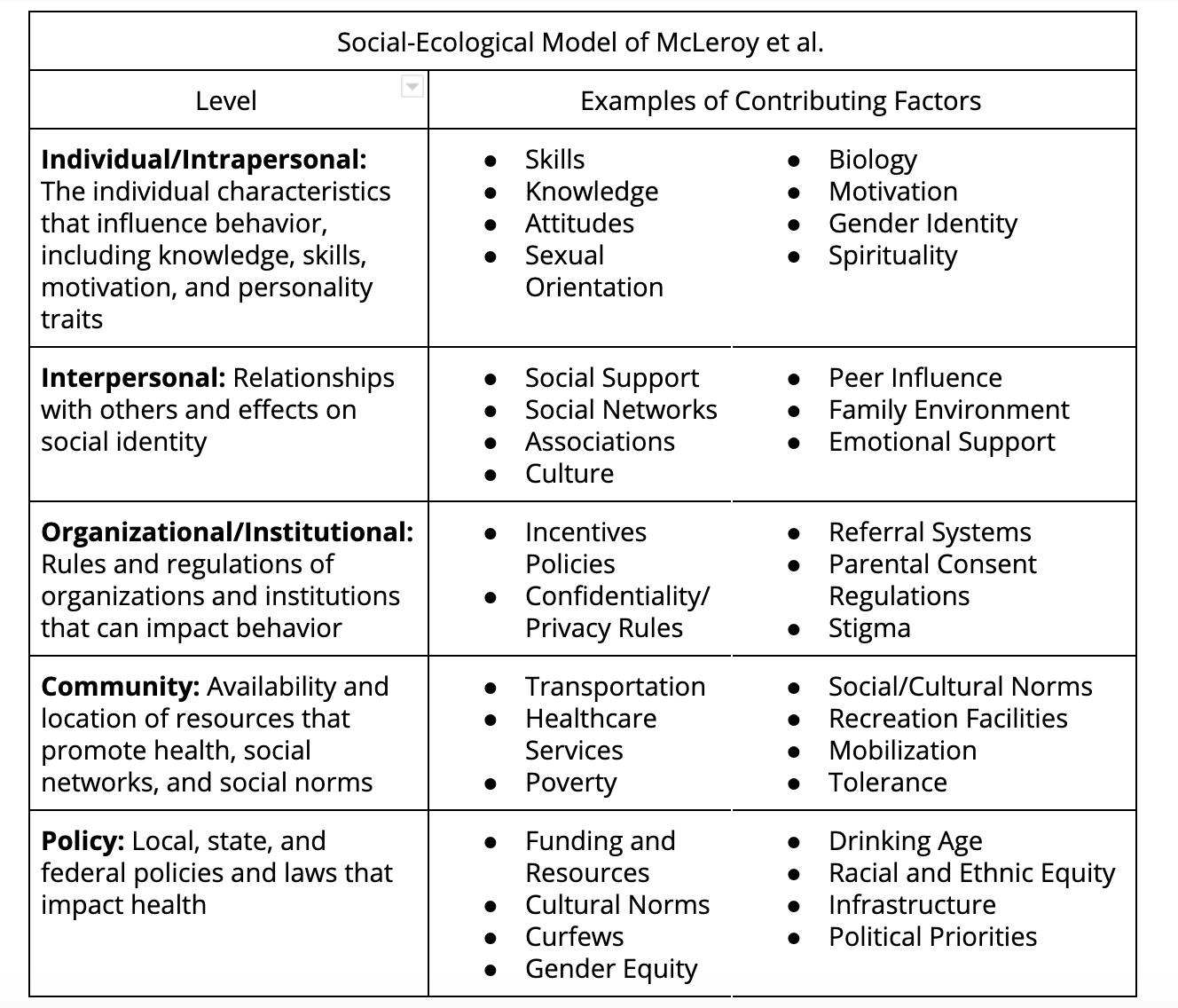
The U.S. Department of Health and Human Services (HHS) frames the SEM perspective as the “interaction between, and interdependence of, factors within and across all levels of a health problem.” The SEM recognizes five levels of influence on health: individual/intrapersonal, interpersonal, organizational/institutional, community, and policy. Essentially, it provides a theory-based framework for understanding exactly how the social determinants of health influence and maintain health and health-related issues.
In the United States, successes in tobacco control have more than halved smoking rates since the 1964 landmark Surgeon General’s report came out warning of the health risks of smoking. Since then, Americans’ view of smoking has changed from an accepted norm in society to a discouraged threat to individual and public health. It was not due to individual interventions targeting one level of the SEM, but a collective effort of stakeholders that touched and influenced all levels of the SEM:
With a multilevel approach, the social and physical environment or community discouraged smoking, and smokers had a better chance of quitting. The drastic shift in smoking metrics highlighted the importance of strong community stakeholder engagement. The communities that had more businesses, workplaces, schools, organizations, and political leaders on board showed the most drastic changes in smoking-related behaviors and outcomes. This public health success story was evidence-based, goal-oriented, and decades in the making. We can learn so much in our work on social determinants from the smoking prevention case study.
After more than one year at Activate Care, a digital health start-up, I have discovered countless ways public health work can be amplified with technology. I have reinforced my understanding that he best chance at sustainable health equity is through community-based initiatives outside the walls of hospitals. The evidence is our innovative partners across the country standing up coordinated systems of care across health and social sectors to more efficiently and effectively address complex issues such as homelessness, substance abuse and mental illness, and many other chronic public health issues. One ongoing project that exemplifies this work is Marin County’s Whole Person Care program in California.
The Whole Person Care approach is building upon existing programs and services by implementing a unified, coordinated entry and care management system; by standardizing screening, assessments, and care coordination; and, by promoting bi-directional information sharing and care coordination among providers. The goal for this systems-level change is new, coordinated, and sustainable approaches to meeting the needs of high-risk, high-cost Medi-Cal beneficiaries.
- Marin Health and Human Services
My public health lens now includes technology and its strengths of data sharing, data tracking, communication, and security, as well as capitalizing on its ability to disrupt traditional care management and social referrals systems. Now more than ever can technology help public health innovators amplify their impact on the most marginalized populations. Although technology has great potential, an engaged community of stakeholders will always be the most important factor for success.
Hear from a former Care Coordinator on how to successfully engage members of the community to achieve better health outcomes at our webinar on August 19. Register now.

One of my most memorable rotations during medical school was a month-long pairing with a late-career general practitioner. He had been using the traditional written...

Our Navigating the Path Storytelling Series introduces the people who make up our incredible community of employees, leaders, partners and patients. Together we help our...