What are the 5 Main Domains of Social Determinants of Health?
The social determinants of health (SDOH) are the multiple, varied factors of where a person lives, works, plays, eats, goes to school, worships, etc., that all combine to impact the quality of life a person can live. Social determinants of health are non-medical factors that influence health outcomes for individuals. Since medical care is estimated to account for only 10-20% of health outcomes for a population, leaving the other 80-90% up to non-medical factors broadly called the social determinants of health, we need to be able to group all of these factors into actionable buckets. Instead of asking what are SDOH, we should ask what the five main domains of the social determinants of health are. This is highly important and valuable work because a meta-analysis of studies using U.S. death data found that the number of U.S. deaths in 2000 attributable to low education, racial segregation, and low social support was comparable with the number of deaths attributable to heart attack, cerebrovascular diseases such as stroke, and lung cancer, respectively.
Promoting healthy behaviors alone can’t eliminate health disparities if we don’t address social determinants of health.
What Are Social Determinants of Health?
There are five major domains of social determinants of health, including these:
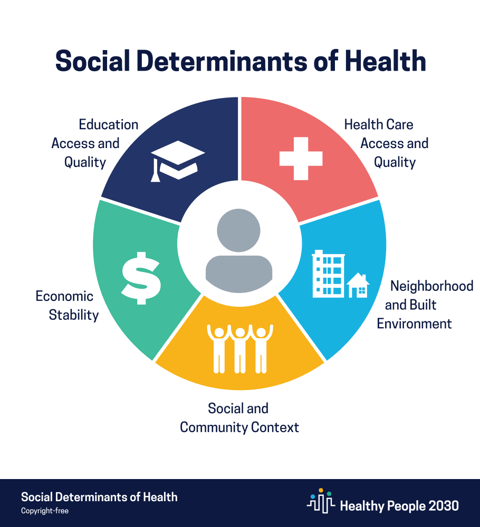
Economic Stability
Economic stability refers to people's income, socioeconomic status, and cost of living, with factors such as poverty, unemployment or underemployment, food insecurity, and housing instability negatively impacting health.
Social and Community Context
Social and community context is often forgotten as a social determinant of health, covering the contexts in which people live, study, work, and relax. The sense of belonging to a community, workplace conditions, and discrimination or racism all impact people's health.
Neighborhood and Built Environment
As a social determinant of health, the neighborhood and built environment affect health outcomes through quality of housing, access to transportation, access to healthy foods and clean water, air quality inside and outside, and the impact of crime and violence on people who live in the area.
Healthcare Access and Quality
Healthcare cannot be left out of social determinants of health, of course. Access to healthcare is not equal, and people's financial and physical access to healthcare, as well as their understanding of health services and their health, is a major social determinant of health. This includes access to primary care, access to specialty care, health insurance coverage, and health literacy. Health literacy is especially salient as a non-medical social factor, for example, whether people know how to prevent painful kidney stones that can be risky to remove surgically by proper diet and staying hydrated—things people know they “should” do. Yet, it’s difficult to attach importance to it without knowing why.
Education Access and Quality
Education also influences health and well-being. Education factors include early childhood education and development, graduating from high school, receiving higher education, and even English knowledge and literacy.
What Stands in the Way of Social Determinants of Health Interventions?
Earlier this year, at the RISE National conference, Activate Care hosted a roundtable discussion to ask health systems and MCOs the question, “What barriers prevent you from providing proactive SDOH interventions?” These were the major categories of answers:
- Screening is avoided because organizations don’t have the resources to address the risks they would uncover.
- Screening is avoided because there’s always something more immediate, urgent, and higher risk right now that needs to be addressed in the short clinical visit time.
- Screening is occurring, but finding more SDOH needs than the health system or payer is equipped to deal with through a shortage of resources, bandwidth, or care coordination ability.
- The lack of a single dataset on SDOH interventions provided through disparate care partners makes it difficult to prove interventions are effective and save money.
In other words, organizations interacting with folks experiencing SDOH and health-related issues don’t have dedicated staff resources to work with them beyond their main specialty. They have limited time to address multiple disparate needs of the person, have a lack of knowledge or lack of available resources to help the person, and have a lack of coordination across the community as there isn’t a system to track and provide support centered on the person, not the individual organizations. It can seem impossible to adequately address and manage high numbers of clients with SDOH needs. Even if those needs are met, it can be hard to show an intervention is working and should continue to be financially incentivized or should receive reimbursement or quality payments. Data for one person with three SDOH needs, for example, housing, food security, and non-food needs like diapers or hygiene products, can end up scattered across three silos unconnected from the doctor’s office, health system, or payer. You need support and systems to help drive these efforts and improve your community’s outcomes.
An Innovative, Proactive Approach to Addressing SDOH Will Help
To address SDOH proactively, organizations must engage with people before they are in crisis and have an avoidable event - leading to high-cost, unnecessary medical care. To accomplish that, you need to have a model in place with dedicated staff resources tasked with helping to navigate people along that path to care. Care Coordination is a hard problem to take on alone, especially with all the challenges MCOs, health systems, payers, and communities already face. Partnership with Activate Care is another way that MCOs and healthcare systems can help meet social determinants of health needs.
Activate Care connects individuals to services that can help them improve their social determinants of health, closing the gap on resulting health disparities. For example, Activate Care has helped reduce chronic homelessness by 28%, increased patient engagement, and reduced avoidable hospital admissions for clients by 21%.
Health equity can be improved by identifying people’s social determinants of health needs, connecting them to the right services, and coordinating care to ensure that the resources people have been referred to are actually reaching them and improving their lives.
Are you a member of a community or organization that could benefit from improved care coordination across multiple organizations? Learn more about Activate Care’s Path Assist solution.