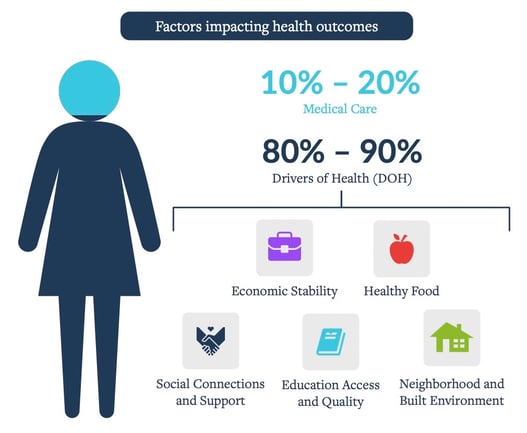
The United States pays more for medical care than any other high-income nation, yet has the worst health outcomes. In fact, the U.S spends the highest proportion of its gross domestic product on health care, according to the Commonwealth Fund. How and where we direct our healthcare spend needs to change. Currently, 90% of health spend is allocated to medical care, which only directly influences 10-20% of health outcomes, while 80-90% of a person’s well-being is driven by the social determinants of health (SDOH) they face on a daily basis. We need to be proactive in our approach.
Addressing health issues and the factors outside of the health system that lead to poorer outcomes is a crucial part of solving healthcare. Proactive outreach, such as using trusted community health workers and navigators is a step forward, along with having useful, actionable data and personalized care plans. Keeping people out of the hospital and having earlier interventions is the only way to keep our systems sustainable.
So how do we get there? There is a significant opportunity to make an impact if we focus on how we address SDOH, specifically, how we could transition from a reactive to a proactive approach.
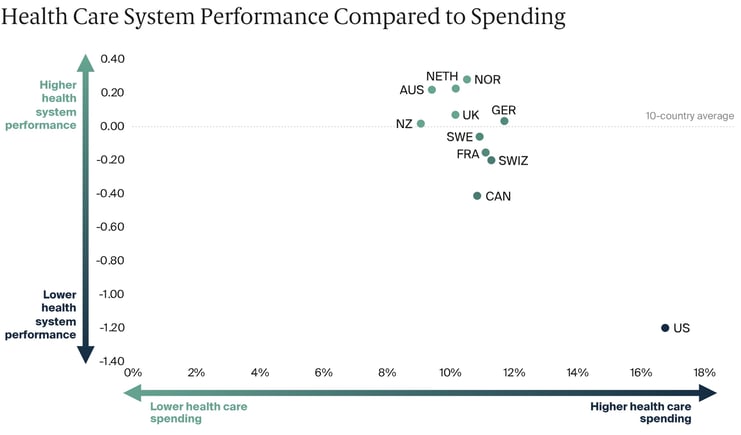
Source: https://www.commonwealthfund.org/publications/fund-reports/2021/aug/mirror-mirror-2021-reflecting-poorly
Non-Clinical Drivers of Health
The drivers of health (DoH) account for 80 percent of health outcomes and have a disproportionate impact on communities of color, including “stable, affordable housing; healthy food; reliable income; and interpersonal safety, among others.” Having a proactive, whole-person care approach can help address these needs and care gaps.
We can prevent a patient from needing an ER visit and receiving costly health care, by having earlier interventions - not only once they already need medical care. If we address SDOH proactively, identifying risks before they become larger problems, we allow people to have a better chance at a healthy life.
Engagement + Improved Outcomes
Findings of a 2019 study revealed a strong link between SDOH and the development of chronic disease. US adults with an increasing number of social risk factors were progressively less likely to attain ideal levels of cardiovascular health factors. A MedCity conference discussion highlighted how people often have overlapping SDOH that are the root cause of their medical issues.
A 2019 study found that food insecurity (an SDOH) – which can lead to diabetes, heart disease, and other chronic conditions – costs the health system an additional $53 billion annually. Change requires getting people to resources and helping them through a sometimes complex and confusing system. Our CHNs provide that one-on-one support and help guide members through the systems and barriers they face. It’s not enough to offer service if a member isn’t an active participant in their care - we help enable that.
Source: CHRISTENSEN INSTITUTE: YOU ARE WHAT YOU TREAT
Community Care
Community Health Workers (CHW) help serve as an extension of the work already being done at the community level. CHWs can help ease the burden placed on an over-fatigued healthcare community. Driving meaningful change to directly impact lives requires trusted community members with lived experience in the community to provide guidance and education - and to empower people to get the services available to them. In our collective drive towards health equity, we can’t afford to treat people once it’s too late.