I recently had the pleasure of hosting a teleconference with the Scottsdale Institute and Activate Care customer Queen of the Valley Hospital in Northern California. The Scottsdale Institute is a not-for-profit membership organization of prominent healthcare systems who support their members’ efforts to achieve clinical integration and transformation through information technology.
Queen of the Valley is part of Providence St. Joseph Health, a healthcare system created by Providence Health & Services and St. Joseph Health with the goal of improving the health of the communities they serve, especially those who are poor and vulnerable. For this webinar, I was joined by Providence St. Joseph’s Dana Codron, RN, MPH, Northern California Regional Director for Community Health Investment, as well as Aura Silva, RN, PHN, Manager of the CARE Network for Queen of the Valley.
Queen of the Valley’s CARE Network - which stands for Case Management, Advocacy, Resources, and Education - serves vulnerable patients with complex health conditions by offering community-based medical and psychosocial care management. The CARE Network is made up of a team of registered nurses, social workers, community health workers, and behavioral health specialists who work together to address the root causes of poor health for their patients and improve their patients’ health outcomes and quality of life. Part of this network also includes a mental health team to assist patients with mental health issues and overcome the mental health-related barriers that stand in the way of treating their health issues.
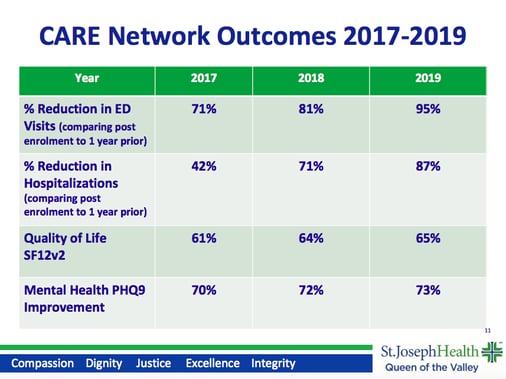
The CARE Network, led by Aura Silva, has achieved nothing short of amazing results, year after year. One thing that sets Aura and her team apart from other interventions is that they're really good at measurement and evaluation. According to their internal data, they are able to achieve huge reductions in ED visits and hospitalizations in just one year, post-enrollment. According to an external study, before enrollment, patients had a mean cost of care of over $5,000 per member per month (PMPM). During the middle of this study - post-enrollment - this mean cost of care drops to $2,500 PMPM. After the study ended, for those same individuals that they could track, it was down to $1,300 PMPM. Simply put, the CARE Network provides an individualized care management program that has a true population health impact for the most vulnerable populations.
How do they achieve these results - and how can you follow their lead?
The CARE Network often sees patients who use the emergency room for primary care. Some individuals have as many as 50 ED visits per year when they enroll in the CARE Network program. They may have language barriers and lack English. As many as 1,200 CARE Network clients live below the poverty level at any point in time. Approximately 75% of clients are Medicaid beneficiaries. These patients encounter multiple barriers to accessing appropriate care and services, but as Aura and her team work with them, they help break down these barriers.
Many of the patients they see are often homeless or housing unstable and have multiple chronic conditions. Often with the lack of financial resources and social support, these individuals struggle with managing their health conditions on top of social isolation and housing and food insecurity they’re experiencing.

The CARE Network’s interdisciplinary, community-based model has evolved over the past 20-30 years. Due to the life challenges of their clients, the care team has a big initial focus on social work. The nurse care manager’s initial focus is helping them get their medications. A community health worker serves as navigator and provides needed supports to ensure resources are accessed; this allows the social worker and nurse to work to top of license. In 2010, they added behavioral health resources to the team, as behavioral health needs create significant barriers to optimal management of chronic diseases. Like much of the country, they had also seen an increase in substance use disorders, especially related to opioids.
All of CARE’s social workers are certified in SOAR (SSI/SSDI Outreach, Access, Recovery). With this certification, they know how to help clients navigate the Social Security benefits process. Across the country, this population of clients would not normally be approved for social security after their first application. The initial approval rate is just 10% nationwide. By following the SOAR process, our team helps to achieve a success rate of 55-60%. It’s one small step in the right direction for this vulnerable population.

Only about 50% of CARE’s referrals come from the medical center. All other referrals come from community partners, including various community-based organizations, county services, and other healthcare providers. Every referral begins with the Intake social worker who determines the program and care team that best fits the individual’s needs. A psychosocial assessment leads to the individualized care plan, which is developed with input from the client. They specifically ask the client what they want to work on, and make an effort to set aside the health system’s priorities in order to ensure they’re meeting the client where they’re at.
It takes, on average, six months to one year to develop and deliver the care management process, but it is not uncommon for clients to receive services for longer than a year. Over time, the CARE Network convenes multidisciplinary team meetings with participation from various community agencies, which allows them to maintain a comprehensive community approach. Their partners often include adult protective services, mental health providers, drug and alcohol services providers, probation officers, and local FQHCs - essentially, everyone who can help come up with a plan for that client’s needs.
How Activate Care helps
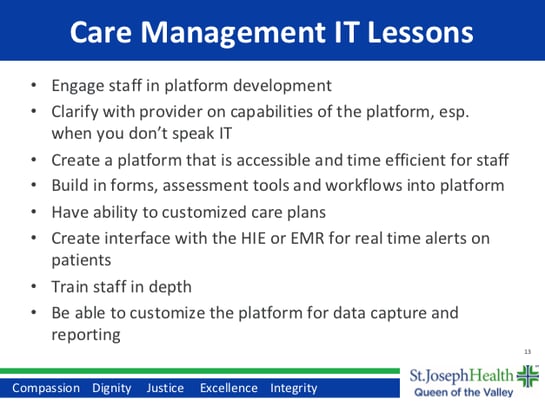
Two years ago, Queen of the Valley started looking for a tailored software platform for the CARE Network. Their contracts with various funders required specific IT needs, including the ability to produce individualized care plans, specific documentation and workflows, assessments, reports, and other contract deliverables. Their search led them to Activate Care’s solution, the Activate CareHub™ platform.
Even being part of a large health system, their EHR does not have the capabilities needed to develop and execute individualized care plans reflecting patient goals and priorities, or tools to track activities of care and take in patients across the community, or track new and unique data to inform and drive process improvement. Ultimately, it was the ability to customize care plans that was so important to Aura and her team, so they could always see where the patient was at, and adjust it to meet evolving patient needs.
Get in touch
Since 2013, Activate Care’s tools have been used by thousands of professionals like Aura and Dana to improve the effectiveness, quality, and safety of their community care coordination programs. If I can help answer any questions or give you a look at the platform, you can always reach me at dave@activatecare.com.
Join us for our upcoming webinar and discover how organizations like yours can become leaders of referral networks, and how leaders can refocus referral management programs around community coordination.
