The association between social drivers of health (SDOH) and health outcomes is well-known and documented, and there is a widespread consensus that resolving health-related social needs (HRSNs), such as food security, transportation access, and stable housing, can lead to improved health outcomes. However, the large and growing body of literature around designing and evaluating interventions that address HRSNs rarely describes the precise mechanisms that lead to the intended outcomes.
The figure below illustrates the foundational mechanisms that shape the Path Assist program, our internally developed social needs intervention. The interplay between individual and environmental factors that influence health outcomes is too complicated to fully cover in a short post, so we have restricted our focus to the factors most relevant to our intervention. In the remainder of this post, we will unpack this diagram by giving an overview of how each of the intervention’s three core activities—social needs screening, resource navigation, and behavioral coaching—leads to positive impacts for our clients, their communities, and the health plans that insure them.
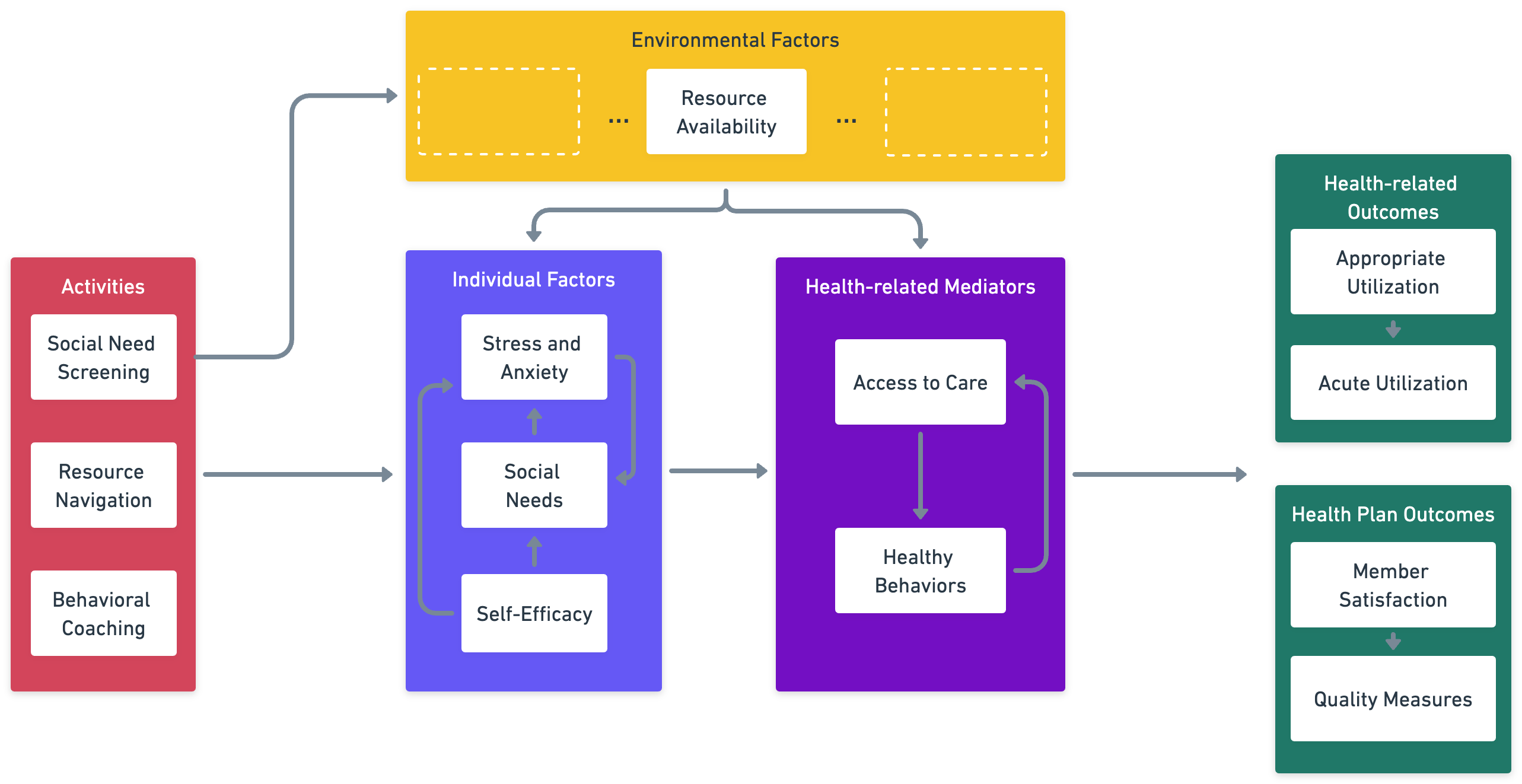
**Other environmental factors are critical, but not explicitly included in this diagram because they are not hypothesized to be directly impacted by our intervention.
Path Assist is a community-based, community health worker (CHW)-led social needs intervention designed to impact both psychosocial and health-related outcomes. Prior to launching the intervention in new geographies, we engage individuals and organizations in those communities through a community assessment to better understand the community’s demographics and health disparities, unique strengths and challenges, leading SDOH factors, as well as barriers and facilitators to care. This work informs how we deliver the intervention in that particular context and lays the foundation for stronger community engagement, agency collaboration, and resource allocation. While we do not treat the community assessment as an independent intervention activity in this post, it is essential to the overall success of the intervention in that it bolsters every pathway.
Social Needs Screening
Screening for HRSNs is foundational to the other pathways and provides a distinct pathway to achieve positive health outcomes in the long term. Most directly, screening increases awareness of the prevalence and severity of unmet HRSNs at both individual and population levels. At the individual level, screening provides the CHW with a starting point to offer client-centered care and support to directly remediate client-identified needs.
At the population level, increased needs awareness may lead to additional social services funding, expanding the pool of available resources. This part of the pathway is not only theoretical but also eminently practical. For example, Fitchenberg, Alley, and Mistry (2019) noted that screening has led multiple health systems to make substantial investments to improve access to housing programs and quality food sources. Additional resources, in turn, allow more social needs to be met. Screening for social needs is a catalyst to the second pathway we will discuss, resource navigation, by mitigating one critical environmental barrier: the lack of available social resources.
Resource Navigation
Resource navigation supports an individual in accessing local, trusted, and appropriate resources or services that can help resolve or lessen the burden of their specific unmet HRSNs. This process involves providing referrals to relevant resources and supporting individuals in connecting with those resources. Resource navigation positively impacts health outcomes through multiple pathways.
Consider an individual motivated to engage in healthy behaviors, such as eating well, exercising, and attending routine medical exams. However, this person lives in a neighborhood with few resources within walking distance and limited options for public transportation, and he has no access to a personal vehicle. The retail conditions in his neighborhood make it hard for him to buy healthy food, and his lack of transportation makes it difficult to get to a clinic regularly.
While this is a specific example, the same logic applies to resolving any HRSN. By definition, HRSNs act as barriers to engaging in healthy behaviors and accessing health care. Therefore, resolving these needs can directly impact individuals’ well-being and long-term health outcomes.
Resource navigation that resolves HRSNs also impacts health outcomes by reducing stress and anxiety. Elevated stress over long periods of time has harmful effects on health outcomes; therefore, reducing stress can directly improve health. Reducing stress improves health outcomes through two additional pathways. First, there is a virtuous cycle between reducing stress and resolving HRSNs; resolving a need reduces stress, making it easier to resolve other needs, further reducing stress and ultimately compounding the positive health effects. Second, reducing stress increases an individual’s ability to engage in health-promoting behaviors, which leads to improved health outcomes.
One major challenge associated with these pathways is that successful resource connection via a closed-loop referral that culminates in need resolution is mediated by a multitude of individual and environmental factors beyond the CHW’s control. These factors lead to highly variable and often lower connection rates than expected. For example, reported resource connection rates range from 10% (Schickerdanz et al., 2019) to 50% (Renaud et al., 2023). Despite these wide-ranging and often low connection rates, there is substantial evidence that social needs interventions can have positive health outcomes, particularly around reducing emergency department (ED) utilization.
For example, Kelley et al. (2020) found that an intervention targeting Medicaid-insured frequent ED users had 1.4 fewer visits to the ED in the year following the intervention. This positive evidence implies that there may be alternative pathways to achieving positive health outcomes, regardless of whether needs are ultimately resolved. As we discuss next, one plausible pathway is through the behavioral coaching techniques that CHWs employ to enable their clients to not only solve their immediate needs but also equip them to overcome challenges in the future. Through this mechanism, positive health outcomes can be achieved independent of whether HRSNs are fully resolved.
Behavioral Coaching
Behavioral coaching involves a client-centered approach to goal-setting, action-planning, and boosting confidence to achieve behavior change. Ultimately, coaching can lead to higher rates of needs attainment, deeper trust, sustained behavior change, and a longer-lasting positive impact of the intervention. In the short term, the trusted relationship between the client and CHW can also allow the individual to feel supported, which can directly reduce their stress and anxiety levels. Again, this is not just a theoretical pathway but one we regularly hear articulated by Path Assist participants. One client described the CHW’s impact on him this way:
It's nicer when you have somebody helping you navigate through these problems. I felt alone and stuck and, and, you know, working with my CHW, you know, there were still a lot of times I still felt that way, but when she would call, that feeling would go away.
CHW-led coaching equips individuals with skills and strategies that increase their capacity to solve new problems. This increase in self-efficacy facilitates engaging in health-promoting behaviors like adhering to prescribed treatment (Roncoroni et al., 2019) that lead to improved health outcomes.
Impacts on Health Outcomes
Although we have primarily focused on the positive impacts on participants thus far, Path Assist can also positively impact the health plans that insure these individuals in three ways:
- By screening individuals for HRSNs and providing a tailored intervention as needed, Path Assist directly impacts quality scores like the HEDIS SNS-E measure, which quantifies the degree to which a health plan screens for social needs and administers an appropriate intervention promptly (e.g. 30 days).
- Path Assist can impact the total cost of care by reducing participants’ dependence on emergency departments for non-emergent healthcare and non-health-related needs. Each of the three core intervention activities engages pathways that reduce both psychosocial and health-related barriers to care. By mitigating these barriers, Path Assist enables clients to engage in healthy behaviors, access appropriate healthcare services, and reduce dependence on acute care services, except when necessary.
- We have a robust outreach process for identifying, recruiting, and retaining eligible members for Path Assist.
Engagement with Path Assist translates to higher engagement with the health plan, leading to higher retention rates and improved quality scores for the plan.
In this post, we have outlined the major pathways by which Path Assist, our social needs intervention, improves outcomes for individual participants, their health plans, and their communities. These pathways are fundamentally driven by non-health-related activities, including screening, resource navigation, and behavioral coaching. However, we have confidence in Path Assist’s ability to affect health-related outcomes due to the well-known interplay between biological, psychological, social, and health-related factors contributing to health outcomes. While the interplay between these factors is more complicated than what we have addressed in this post, we hope that the core mechanisms by which it operates are clear and compelling. For additional information about the Path Assist program, please complete this brief form.